
• Renal function is often assessed using BUN, Cr, and GFR values routinely measured as part of chemistry panel.
• Additional tests can be obtained to further assess renal function-- those include urine chemistry (e.g. urine Na, Cr, protein, osmolality) and urine microscopy (e.g. presence of rbc, wbc, epithelial cell, cast, crystal, or other urine ediments).
• BUN and Cr are metabolites excreted by the kidneys (as illustrated below) thus their accumulation in the blood suggests poor renal function.
• BUN level is also affected by protein level in the blood (which is elevated in high protein diet and upper GI bleed).
• Cr level is also affected by muscle mass, muscle breakdown, and protein intake.

azotemia
• Azotemia refers to the elevation of BUN and/or Cr in the blood.
• Azotemia often suggests decreased GFR (impaired renal function) due to prerenal, postrenal, or intrarenal causes.
• However, not all azotemia cases are renal-related:
BUN also elevates when the urea production in the gut increases (e.g. high protein diet, upper GI bleed)
Cr also elevates when the release of Cr from skeletal muscle increases (e.g. high muscle mass, high protein diet, crush injury)
BUN decreases when the urea production in the gut decreases (e.g. cirrhosis) or the body protein decreases (e.g. low protein diet, starvation)
Cr decreases when the release of Cr from skeletal muscle decreases (e.g. low muscle mass, muscle wasting)
✿ Increased gut urea production
✧ high protein diet
✧ upper gi bleed
✿ Decreased glomerular filtration
✧ any intrinsic renal causes
✧ pre-renal causes
⁎ hypovolemia
⁎ hypotension
⁎ sepsis
⁎ heart failure
✧ post-renal obstruction
✿ Decreased total body protein
✧ low protein diet
✧ starvation
✿ Decreased liver urea production
✧ cirrhosis
✿ Increased glomerular filtration
✧ osmotic diuresis (hyperglycemia)
✿ Increased release from muscles
✧ high muscle mass
✧ high protein diet
✧ increased muscle breakdown
⁎ crush injury
✿ Decreased glomerular filtration
✧ any intrinsic renal causes
✧ pre-renal causes
⁎ hypovolemia
⁎ hypotension
⁎ sepsis
⁎ heart failure
✧ post-renal obstruction
✿ Decreased release from muscles
✧ low muscle mass
⁎ women
⁎ elderly
✧ muscle wasting
⁎ cachexia
⁎ sarcopenia
✿ Increased glomerular filtration
✧ osmotic diuresis (hyperglycemia)
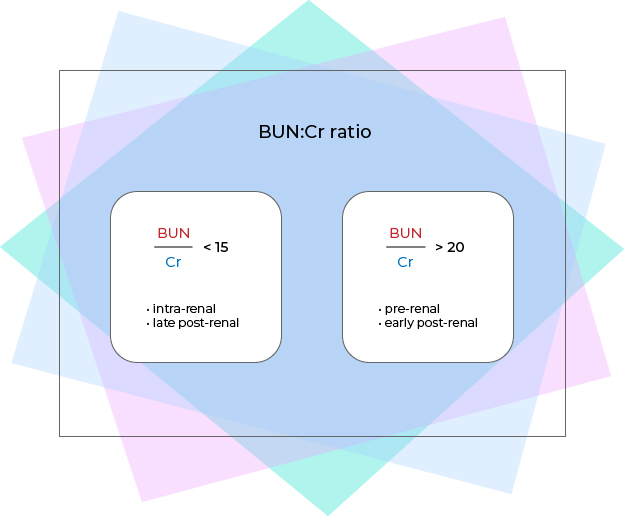
BUN:Cr ratio
• BUN/Cr ratio is used to further determine whether the renal cause of azotemia is prerenal, intrarenal (intrinsic), or postrenal.
• If BUN/Cr ratio is < 15, BUN and Cr are elevated proportionately with each other, meaning both the filtration rate (affected by blood flow) and the kidney tubules are abnormal-- which are caused by intrinsic renal injury or late (long standing) post-renal injury leading to tubular damage.
• If BUN/Cr ratio is > 20, BUN are much more elevated than Cr, meaning kidney tubular function is normal (Cr level only slightly elevated) but there is a decrease in filtration rate due to decreased blood flow in the case of pre-renal injury. Early post-renal obstruction does not cause damage to the kidney tubules but the slowered urinary flow allows more urea to be reabsorbed thereby increasing serum BUN level.
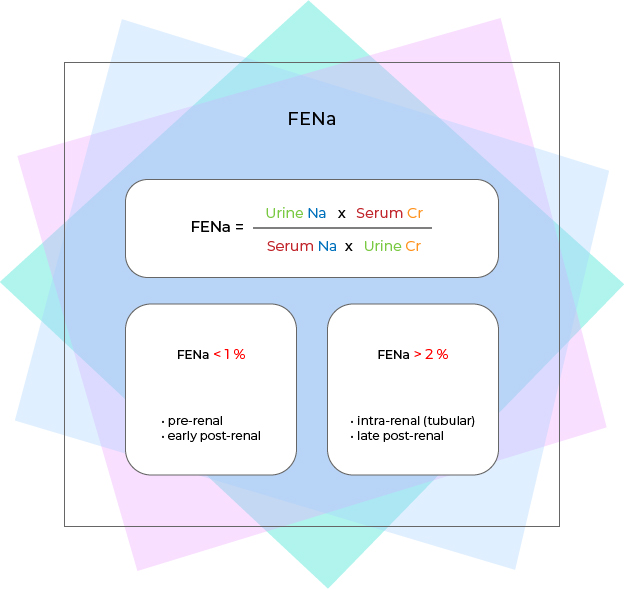
fena
• In addition to BUN/Cr ratio described above, FENa (Fractional Excretion of Na) is another tool used to determine whether the renal cause of azotemia is prerenal, intrarenal (intrinsic), or postrenal.
• FENa is calculated by mutiplying the ratio of urine Na over serum Na by the ratio of serum Cr over urine Cr.
• If FENa is < 1%, Na reabsorption/excretion remains appropriate thus suggesting relatively intact renal tubules-- this is seen in prerenal and early postrenal diseases.
• If FENa is > 2%, Na reabsorption/excretion is impaired (higher urine/serum Na ratio reflects Na overexcretion/ impaired Na reabsorption) thus suggesting damaged renal tubules-- this is seen in intrinsic (mostly due to tubular diseases) and late postrenal diseases.
acute kidney injury
• Acute kidney injury (AKI) is defined as an elevation in serum creatinine and/or a decline in urine output.
• There are three major AKI patterns: prerenal, intrarenal (intrinsic), and postrenal:
Prerenal: decreased renal blood flow or change in renal arteriolar resistance leading to decreased GFR
Intrarenal: tubular, interstitial, or glomerular damage leading to impaired renal function
Postrenal: ureteral, bladder, or urethral obstruction leading to increased hydrostatic pressure inside renal tubules and decreased GFR
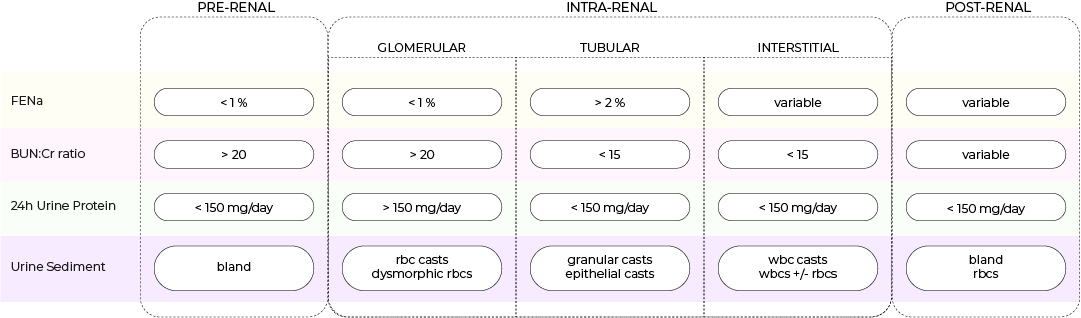
• Lab findings associated with differents AKI patterns are summarized in the table below. Key findings for each pattern are:
Prerenal: has high BUN:Cr ratio and low FENa, no proteinuria, normal urine sediment
Postrenal: has variable BUN:Cr and FENa, no proteinuria, and urine sediment can be bland or has red blood cells (obstructive uropathy)
Intrarenal (glomerular): causes proteinuria and rbc casts with dysmorphic rbcs in urine sediment but has high BUN:Cr ratio and low FENa
Intrarenal (tubular): has high FENa and granular or epithelial casts in urine sediment, often without proteinuria
Intrarenal (interstitial): has variable FENa and wbc casts with wbcs or rbcs in urine sediment, most often without proteinuria
✿ Hypovolemia
✧ hemorrhage
✧ gi losses (diarrhea, vomiting)
✧ renal losses (diuretics, hyperglycemia)
✧ insensible losses (sweat, hyperventilation)
✿ Low effective circulating volume
✧ shock
✧ sepsis
✧ heart failure
✧ cirrhosis (hepatorenal syndrome)
✧ acute pancreatitis
✧ severe burns
✿ Altered renal arteriolar resistance
✧ afferent arteriolar vasoconstriction
⁎ nsaids
⁎ calcineurin inhibitors
⁎ iv radiocontrast
✧ efferent arteriolar vasodilation
⁎ ace inhibitors / arbs
✿ Interstitial causes
✧ acute interstitial nephritis
✲ drug-induced
⁎ nsaids
⁎ antibiotics (penicillin, cephalosporin)
⁎ proton pump inhibitors
✲ infection
✲ infiltration
⁎ malignancy
⁎ sarcoidosis
✲ autoimmune
✲ idiopathic
✿ Glomerular causes
✧ rapidly progressive glomerulonephritis
⁎ goodpasture's syndrome
⁎ IgA nephropathy
⁎ systemic lupus erythematosus
⁎ poststreptococcal glomerulonephritis
⁎ mixed cryoglobulinemia
⁎ wegener granulomatosis
⁎ churg-strauss syndrome
⁎ microscospic polyangiitis
✧ nephrotic syndrome
⁎ minimal change disease
⁎ focal segmental glomerulosclerosis
✿ Tubular causes
✧ acute tubular necrosis (atn)
✲ ischemic atn
⁎ prerenal azotemia (shock, sepsis)
⁎ renal artery thromboembolism
⁎ renal artery dissection
⁎ microangiopathy (dic, ttp/hus)
⁎ malignant hypertension
⁎ renal vein thrombosis
⁎ abdominal compartment syndrome
⁎ nutcracker syndrome
✲ toxic atn
⁎ antibiotics (aminoglycosides)
⁎ antifungals (amphotericin b)
⁎ antivirals (acyclovir, foscarnet)
⁎ chemo (cisplatin)
⁎ immunosuppressants (cyclosporine)
⁎ iv radiocontrast
⁎ heavy metals (lead, mercury, platinum)
⁎ ethylene glycol
⁎ urate (tumor lysis syndrome)
⁎ light chain (multiple myeloma)
⁎ myoglobin (rhabdomyolysis)
⁎ hemoglobin (hemolysis)
✿ Ureteral obstruction
✧ stones
✧ strictures
✧ blood clots
✧ benign or malignant mass
✧ renal papillary necrosis (sloughed papillae)
✿ Bladder neck obstruction
✧ neurogenic bladder
✧ anticholinergics
✧ benign prostatic hyperplasia
✧ prostate cancer
✿ Urethral obstruction
✧ stones
✧ strictures
✧ blood clots
✿ External compression
✧ retroperitoneal fibrosis or mass
✧ cervical cancer